By Johan Marais
Like elsewhere in the world, it’s very difficult to obtain accurate figures for the number of snakebites in Swaziland every year. Thea Litschka from the Swaziland Antivenom Foundation has been visiting hospitals and clinics for many years and at times she hears of as many as 40 bites in one month. But figures for people who are bitten and die before they are admitted to hospital are not available, and this is pretty much the case elsewhere in southern Africa.
Generally speaking the treatment of snakebites is poorly understood in Swaziland, with most doctors, nurses and paramedics having no idea what to do. Antivenom is usually in short supply or far too little is administered in medical emergencies. At times the antivenom is injected intramuscularly or around the site of the bite – a total waste of time and resources.
Most snakebite victims arrive at the hospital with a tourniquet and in many cases, especially Mozambique Spitting Cobra and Puff Adder bites, the consequences of such first aid measures may be devastating. These victims also rely on treatment from traditional healers, and we know that there is no plant or herbal remedy that is effective against the venom of a potentially deadly snake. Not just does this waste a great deal of time but the “muti” that is rubbed into the wound often causes massive infection.
Swaziland currently has no “911” emergency number or poison centre. One vial of antivenom costs close to R1000 and for any serious snakebite emergency where antivenom is administered, anything from 100 – 200 ml (or more) is required. That equates to R10 000 – R20 000 per bite for the antivenom. Because of the costs, few victims receive adequate antivenom and this often results in extended stays in hospitals with multiple sessions in theatre for surgery, daily bandage changes, antibiotics and other medication. This could become very expensive, not to mention the long-term effects on the patient. Most victims are poor farm workers that need their hands and feet to work the land to provide for their families.
Case studies
On such case is Mduduzi, who was fast asleep on his mother’s bed one morning when a Mozambique Spitting Cobra ended up in bed with him. He was bitten on both arms and his mother found him screaming in agony. One of the neighbours killed the snake.
Mduduzi was rushed off to the local clinic where he was given some Panado infant syrup for pain. From there he was taken to a hospital where he received more Panado infant syrup and as they had no antivenom there was very little they could do for him. He spent several weeks in hospital. Antivenom is no guarantee against necrosis but it can be highly effective at reducing the area of necrosis if administered early.
Nathi was also bitten by a Mozambique Spitting Cobra when he went into the kitchen to fetch his grandmother some milk. His brother rushed him to hospital where he received painkillers but again no antivenom. After an extended stay in hospital two fingers had to be amputated.
These, in a bizarre way, were some of the luckier cases. A young girl, who was bitten by a Black Mamba, arrived at the hospital struggling to breathe. There was no antivenom and she died about an hour later. The doctor told her mother to be strong.
A young boy, also bitten by a Black Mamba, was placed on the back seat of a car with his mother and rushed off to the local clinic. The nurse on duty panicked as they had no antivenom and sent them off to the next clinic. They were sent to a third clinic and eventually the father stopped his car and watched his child die.
Education
Thea has been spending a great deal of her time visiting doctors and clinics and doing her best to educate medical practitioners in Swaziland on how to treat snakebite victims. If medical staff can be properly trained in airways management and the correct treatment of snake bites using antivenom when required, most deaths and maiming because of necrosis can be prevented. In the previous year the Swaziland Antivenom Foundation managed to collect just over 250 vials of antivenom and this went a long way to save lives and unnecessary suffering, but ideally they require in the region of 1000 vials.
SWAZILAND SNAKEBITE SYMPOSIUM:
The Swaziland Antivenom Foundation, in conjunction with the Africa Snakebite Institute, will be housing a two day snakebite symposium in Simunye, Swaziland on 12 and 13 October 2013. The purpose of the symposium is to involve as many Swaziland medical practitioners as possible and to educate them on how to manage snakebites. We have secured the services of some of the top snake bite professionals in Africa to present a variety of talks and workshops and we hope to cover as much as possible in the limited time that we will have. Amongst the speakers we have Dr. Darryl Wood from Ngwelezane Hospital – he deals with many snake bites every year; Dr. Colin Tilbury – Colin has worked all over Africa and has published widely on the subject; Dr. Jonathan Pons from Swaziland; Dr. Jenna Taylor from Durban – Jenna is an anaesthesiologist at Albert Luthuli Central Hospital in Durban and has a keen interest in snake bite, Richard Mastenbroek from the Havenziekenhuis Travel Hospital in Rotterdam, Netherlands and Jason Seale from Hartebeespoortdam Snake Park. This symposium will hopefully be the beginning of much bigger things. The Swaziland Antivenom Foundation is hoping to find sponsors to stock all clinics and hospitals in Swaziland – an amount of R860 000 per year is required.
Should you require more information about the symposium or wish to be added to the symposium mailing list, please send me an e-mail. All indications are that the symposium will be very well attended and we will have limited space for non-Swaziland citizens.
SNAKE COURSES:
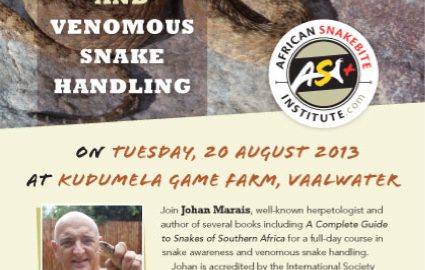
The next available snake awareness and venomous snake handling course will be at Kudumela Game Farm in Vaalwater on 20 August 2013. There will be limited accommodation available at favourable prices. Please e-mail me for more particulars.